Figure 1 – Typical RSA setup for supine (lying down) position (hip, shoulder)

Figure 2 – Typical RSA setup for standing position (knee)

Figure 3 – Uni-planar calibration cage (usually for hip and shoulder exams)
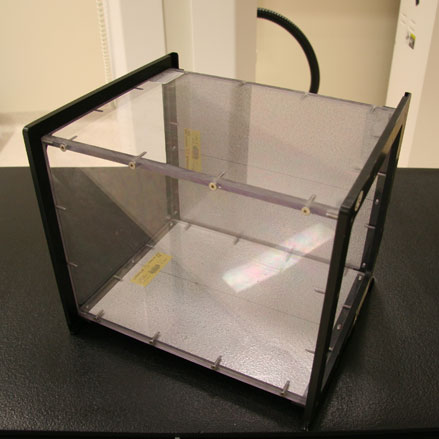
Figure 4 – A biplanar RSA cage for knee joint replacement analysis
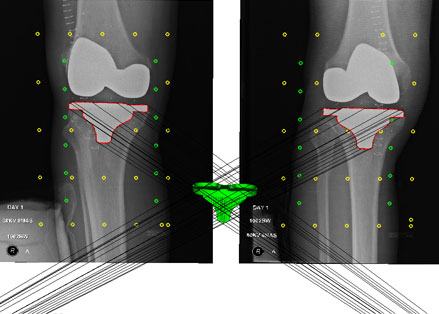
Figure 5 – Pair of RSA Images with analyses.
Radiostereometric Analysis (RSA) was developed by a Swedish researcher, Dr. Goran Selvik, in the mid 70’s as a method for determining an object’s three-dimensional location within a person’s body with extremely high accuracy, up to one tenth of a millimeter.
RSA uses two x-rays which converge on a person’s implant. Much like our vision, we see two individual images from our eyes which our brain combines into one picture, giving us depth perception. RSA is used for studying the migration and wear of many different joint replacements.
During a joint replacement surgery, the surgeon will insert a small number (usually < 10) of tantalum marker beads into the patient’s bone – femur, pelvis, or tibia. Tantalum is a metal that is highly radio-opaque (blocks all x-rays) and therefore appears bright white on an x-ray. These beads are smaller than 1 mm in diameter and are well known to be safe and have no effect on the patients’ implant. These markers are necessary to determine implant-bone motion, also known as loosening.
An RSA examination setup is shown in Figure 1.
The patient is placed above or in front of an RSA calibration cage (Figures 1 & 2). This cage provides the necessary markers to correctly locate the patients’ bone and implant markers in three dimensions. The type of cage depends on the location of the implant.
A uni-planar cage (Figure 3) is mainly used for hip and shoulder examinations but can also be used for knee examinations. A bi-planar cage (Figure 4) is sometimes used for knee examinations.
Two separate images are obtained from an RSA exam (Figure 5). These images are analyzed to determine the relative motion between the beads in the bone and the implant.
RSA is a longitudinal process, meaning that RSA examinations will be performed multiple times for a number of years, often 2 years but up to 10 years. The difference between the initial RSA examination and an examination at 1, 2, or 10 years down the road will determine the distance the implant has travelled into or out of the bone as well as any rotation or tilt of the implant. The amount of motion of the implant is important to be able to predict if the implant may become loose in the future and require a revision surgery.
The predictive ability of RSA is key to many new research studies being undertaken in North America and Europe. Because RSA is so accurate and can predict the outcome of implants (with a degree of certainty), clinical trials of new, untested implants can be performed on a small group of consenting patients with very short follow-up, and still provide the answers that researchers, surgeons, and clinicians need.
The Concordia Joint Replacement Group in partnership with the Orthopaedic Innovation Centre are spearheading the formation of a Canadian RSA Network. This network is made up of 5 Canadian orthopaedic centres with RSA capabilities and was initiated to unite and promote RSA research in Canada for the betterment of patient outcomes and safety in arthroplasty. For additional information, please visit CanadianRSANetwork.com.