When is Arthroplasty used?
Arthroplasty is typically performed when all conservative treatments, such as medications, injections, bracing and therapy, have failed to provide pain relief and improve function and the patient is in an optimal medical condition. Replacing the joint allows it to function more smoothly and with less pain. By reducing the pain, a patient’s mobility and quality of life are usually improved.
When is it done?
After making an incision in the affected joint, the surgeon then cuts away the damaged or diseased bone or cartilage, resurfacing and reshaping the ends of the bones so the joint can be rebuilt.
The surgeon inserts a prosthesis or artificial joint part, which is held in place either by a special bone cement or by the bone growing around it and securing it. Virtually all knee replacements are performed using bone cement, while the majority of hip replacements do not use cement based on the design of the device and features of the patient’s own bone.
How long will it last?
Historically, 90% of joint replacements last longer than 15 years, but this is influenced by the amount of stress placed on the replacement. Younger patients tend to have shorter survival of their joint replacments, presumably due to increased demands placed on the joint. Younger patients may be offered non-traditional implants, such as ceramic, for this reason.
Controlling body weight and discussing activity levels with your surgeon or therapist may increase the lifespan of your new joint.
How do I know if joint replacement is right for me?
If you are experiencing joint pain that has grown unbearable it may be time to make an appointment with your family physician to discuss your options.
Based on your discussion and the results of medical tests, your family doctor will determine whether or not you should be referred to an orthopaedic surgeon.
Click here for questions about your readiness for surgery.
Knee Replacement
When arthritis affects both knees or both hips to a similar degree, replacements of both joints can occasionally be done during the same operation or in two operations spaced closely together. When done at the same time, the operation takes longer and requires a longer hospital stay.
There is more stress on your body with this type of surgery and it is only offered to patients who are physically fit and in very good health. The benefit of this is an overall faster recovery since there is only one hospital stay.
Other patients may be offered a second surgery on the other joint shortly after (3-6 months) the first.

Anatomy of the knee joint
The knee joint, surrounding muscles and tissue are important structures in carrying out day to day activities. The knee joint is a complex hinge formed between the large thigh bone called the femur and the large shin bone, called the tibia, covered by the knee cap or patella.
The main muscles spanning the knee joint include the front thigh muscles or quadriceps and the back thigh muscles, the hamstrings. The knee joint is assisted by the other joints of the leg and pelvis as well as the muscles of the entire lower limb and body’s trunk or core. There are a number of mechanisms that can cause the knee joint to become damaged or weakened, ultimately leading to arthritis.
A revision joint replacement is done to replace a malfunctioning previously implanted joint prosthesis. Also called revision arthroplasty, revision joint replacement is often more complicated with less predictable results than primary or a first time joint replacement.
Because of the many different reasons for which a revision joint replacement may be done, surgery decisions are made on an individual basis. Not all revision joint replacements require the replacement of all parts of the implanted joint. In some cases, parts of the original implant may still be in perfect condition while others may need to be replaced.
Reasons a revision joint replacement may be needed include worn-out implants, implants coming loose from the bone, infection of a replaced joint, and instability or misalignment of an implanted joint. Much of the information applicable to the original (or primary) joint replacement in terms of preoperative, intraoperative, and postoperative care is also true for a revision procedure. However, there are some differences of which you should be aware.
Hospital Stay
The hospital stay for a patient undergoing a revision total joint surgery may be slightly longer than for the original surgery. Hospital stays for the original (primary) total joint replacement average around three days. This compares to 5-7 days for a revision total joint replacement patient.
Blood Loss
As with the original joint replacement, revision total joint replacement is associated with some loss of blood during and immediately following the surgical procedure. The lost blood can be replaced with either: 1) blood that you have donated before the surgery or 2) blood that is donated at an authorized blood bank.
In general, we prefer that patients do not donate their own blood prior to surgery. The blood available through the blood bank is tested with sophisticated and sensitive tests to minimuze the risk of infection. You will be in better physical health if you have not donated blood prior to surgery and your overall risk of transfusion is reduced by not pre-donating blood.
Bone Graft
In revision total joint replacement, a bone graft procedure may be required. Grafting involves the reconstruction of the bone surrounding the implant with new bone. The new bone can either be taken from another location in your own body or from a donor patient.
The decision to use your own bone (called autograft) versus donor bone (called allograft) is usually based upon how much bone is needed. If only a small amount of bone is needed, bone can be obtained from either bone removed during the surgical procedure itself or bone taken from another site (such as the pelvis). For many revision total joint replacement cases, more bone is needed than can be obtained from another site from your own body. When this is the case, donor bone is used.
Similar to blood bank blood, donor bone comes from a certified tissue bank. Certification standards include screening of all donor samples for infectious agents (hepatitis, HIV, e.g.) and the assurance of proper processing so that bone grafts carry the smallest risk possible for use in patients.
Revisions for Infection
In the case of a revision due to infection, depending on the type and extent of infection, you may be told that you need to undergo a 2-stage revision. This involves two surgeries: 1) the removal of the prosthesis and the treatment of the bone to get rid of the infection, and 2) inserting a new prosthesis several weeks later after the infection has been eradicated.
A partial knee replacement or Unicompartmental knee replacement may be done if the arthritic damage is confined to a localized part of the joint. The procedure is similar to a total knee replacement, but with only one side of the joint replaced.
Recovery time is generally shorter following this kind of surgery. If the arthritis is widespread, the ligaments of the knee are not intact or the knee has become stiff, then the partial knee replacement is NOT appropriate, and should not be considered.
Hip Replacement
When arthritis affects both knees or both hips to a similar degree, replacements of both joints can occasionally be done during the same operation or in two operations spaced closely together. When done at the same time, the operation takes longer and requires a longer hospital stay.
There is more stress on your body with this type of surgery and it is only offered to patients who are physically fit and in very good health. The benefit of this is an overall faster recovery since there is only one hospital stay.
Other patients may be offered a second surgery on the other joint shortly after (3-6 months) the first.
Hip fractures are commonly called broken hips. You can break your hip at any age, but the majority of hip fractures occur in people older than 65. As you age, your bones slowly lose minerals and become less dense. This happens more quickly in some people than in others. With dimished balance, strength, reflexes and eye-sight that can all occur with age, elderly patients are at higher risk of falling down and combined with weaker bones, the risk of hip fracture can become quite high.
Once a certain level of bone loss has occurred, a person may be diagnosed with a condition called Osteoporosis. Osteoporosis is a thinning of the bones. The bone loss that creates and occurs in osteoporosis causes a gradual loss of density which weakens bones and makes them more susceptible to a hip fracture.
A hip fracture is a serious injury, as the complications can be life-threatening. Fortunately, surgery to repair a hip fracture is usually very effective, although recovery often requires time and patience.
Depending on the type of fracture that has occurred, the hip can either be “fixed” or “replaced”. Surgery to repair a broken hip is called a fixation where the bones are pinned, plated or nailed together again with metal hardware. With certain hip fracture patterns there is a high risk of a portion of the bone failing to heal and collapsing. In these cases, a hip replacent is generally performed. In the majority of patients, this is performed with a hemiarthroplasty in which only the femoral (thigh bone) side of the hip is replaced. This procedure has less bloodloss, less stress on patients physiology and a reduced risk of dislocation. However, hip fractures increasing are being replaced using total hip replacement in younger, more active patients. In a small number of patients that were unable to walk prior to their hip fracture, consideration may be given to non-operative treatment as performing the procedure will likely not affect their long-term mobility and function.
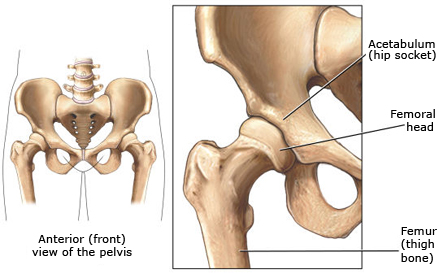
Anatomy of the hip joint
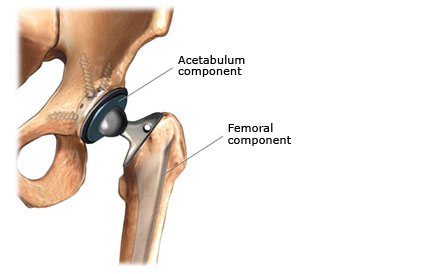
Hip prothesis
The hip joint, surrounding muscles and tissue are important structures in carrying out day to day activities.
The hip joint is a ball and socket formed between the large thigh bone called the femur and the pelvis. The main muscles spanning the hip joint include the hip flexor, extensor, abductor and adductor muscles which help to rotate the hip joint nearly all directions. Movement and support of the hip joint is assisted by the other joints of the leg and pelvis as well as the muscles of the entire lower limb and body’s trunk or core.
There are a number of mechanisms that can cause the hip joint to become damaged or weakened, ultimately leading to arthritis. Arthritis is damage to the boney surfaces that form the joint. It causes pain, stiffness and deformity. Arthritis of the hip makes it difficult walk, get up from a chair, climb stairs,get in and out of bed and tie your shoes, among other activities. As it worsens, arthritis can even cause pain at rest or at night. Arthritis can be hereditary or caused by injury or obesity, however its affects can be lessened by a healthy and active lifestyle.
Hip replacement involves removing the damaged surfaces of the hip joint and replacing them with artificial components called prostheses. With the aid of rehabilitation, a hip replacement can result in reduced pain, improved mobility, strength and function resulting in a better quality of life.
esearch has shown that joint replacement is very effective at achieving these outcomes in most people. For persons who are physically and emotionally ready for Joint Replacement, there is roughly a 90% chance of being satisfied with the outcomes of surgery. For the remaining 10% there are some known and many unknown reasons for less than ideal results.
Complications such as infection or blood clots do occur in less than 1% of patients and can lead to less than ideal surgical outcomes and prolonged recovery. Other important factors such as realistic expectations and sufficient recovery of function are also very important.
It is important to understand your particular risk level for surgical complications and what you can expect after surgery along with the efforts you will undertake to restore your quality of life. Talk to your surgeon about your risk levels, expectations and rehabilitation as it will assist with your decision making for surgery.
A revision joint replacement is done to replace maljuntioning previously implanted joint prostheses. Also called revision arthroplasty, revision joint replacement is often more complicated with less predictable results than primary (first time) joint replacement.
Because of the many different reasons a revision joint replacement may be done, surgery decisions are made on an individual basis. Not all revision joint replacements require the replacement of all parts of the implanted joint. In some cases, parts of the original implant may still be in acceptable condition while others may need to be replaced.
Reasons a revision joint replacement may be needed include worn-out implants, implants coming loose from the bone, infection of a replaced joint, and instability or misalignment of an implanted joint. Much of the information applicable to the original (or primary) joint replacement in terms of preoperative, intraoperative, and postoperative care is also true for a revision procedure. However, there are some differences of which you should be aware.
Hospital Stay
The hospital stay for a patient undergoing a revision total joint surgery may be longer than for the original surgery. Hospital stays for the original (primary) total joint replacement average around three days. This compares to 5-7 days for a revision total joint replacement patient.
Blood Loss
As with the original joint replacement, revision total joint replacement is associated with some loss of blood during and immediately following the surgical procedure. The lost blood can be replaced with either: 1) blood that you have donated before the surgery or 2) blood that is donated at an authorized blood bank.
In general, we prefer that patients do not donate their own blood prior to surgery. The blood available through the blood bank is tested with sophisticated and sensitive tests to minimuze the risk of infection. You will be in better physical health if you have not donated blood prior to surgery, although in major hip revision cases you may be asked to pre-donate blood if large amounts of bleeding are expected.
Bone Graft
In revision total joint replacement, a bone graft procedure may be required. Grafting involves the reconstruction of the bone surrounding the implant with new bone. The new bone can either be taken from another location in your own body or from a donor patient. The decision to use your own bone (called autograft) versus donor bone (called allograft) is usually based upon how much bone is needed.
If only a small amount of bone is needed, bone can be obtained from either bone removed during the surgical procedure itself or bone taken from another site (such as the pelvis). For many revision total joint replacement cases, more bone is needed than can be obtained from another site from your own body. When this is the case, donor bone is used.
Similar to blood bank blood, donor bone comes from a certified tissue bank. Certification standards include screening of all donor samples for infectious agents (hepatitis, HIV, e.g.) and the assurance of proper processing so that bone grafts carry the smallest risk possible for use in patients.
Revisions for Infection
In the case of a revision due to infection, depending on the type and extent of infection, you may be told that you need to undergo a 2-stage revision. This involves two surgeries: 1) the removal of the prosthesis and the treatment of the bone to get rid of the infection, and 2) inserting a new prosthesis several weeks later after the infection has been eradicated.
Your Journey to Surgery and Beyond
Once you and your family doctor decide it is time to consult a surgeon, you will begin your surgical journey. If you and your surgeon determine that joint replacement is right for you, you will begin to follow a “care path”.
A care path or pathway is a specific plan that outlines the activities (by patient and health care staff) that are required on your journey. The surgical care path outlines everything that happens starting with your pre-admission visit, to your day of surgery, to your discharge. The period of time after discharge from hospital is referred to as Rehabilitation.
The care path helps to ensure your recovery progresses in a timely and coordinated manner.
Benefits of the Care Path
- A team approach to quality health care.
- Encourages you and your family to participate in the plan of care and promotes satisfaction.
- Increases your and your family’s awareness of the course of treatment and goals.
- Standardized important educational activities.
- Encourages quick and efficient use of services.
The care path helps track your progress and allows you to be more involved in your care.
The success of your surgery is 20% dependent on the surgeon and 80% dependent on YOU! Be an active participant by discussing your expectations, voicing your concerns and sharing your goals.
Before Surgery
In the weeks prior to surgery, you will be contacted by the pre admission clinic (PAC with an appointment. When attending your PAC visit bring:
- All medications in their original containers (including vitamins and herbal products)
- Magazine/ book (visit may be 1 to 4 hours long)
- Specific questions you may have about your surgery
At the clinic you may be seen by one or several of the following health care providers:
Nurse
The nurse will go over your medical history and answer any questions you may have about the surgery and the hospital stay.
Anaesthesiologist
A member of the anaesthesia team will examine you and discuss the different types of anaesthesia. Further blood work or tests may be ordered.
There may be a need to delay surgery while further tests are done to ensure it is safe to proceed.
**The anaesthesiologist and nurse will go over your medications with you and advise you which medications should be stopped prior to surgery. You will need to stop all vitamins and herbal medications 10 days before your surgery date or your surgery could be cancelled.
Physiotherapist
A physiotherapist will check the movement and strength in your legs, and arms. You will be instructed on exercises to practice before and after your surgery. The therapist will discuss your expectations, lifestyle habits, hobbies and work activities so that you can work together to develop a rehabilitation plan to meet your goals. The therapist will assess your needs for assistive equipment and make suggestions accordingly.
Occupational Therapist
An occupational therapist will discuss changes you will need to make to your home in order to remain safe and follow your movement restrictions. They will also recommend adaptive equipment to make activities of daily living such as getting dressed or bathing easier.
Important information you will receive at PAC:
The Hip and Knee Resource Clinic is designed to provide pre-operative support to hip and knee arthroplasty patients.
The majority of patients will receive their education and optimization from all the clinic disciplines via group educational sessions and by the use of educational materials such as booklets and videos.
There will occasionally be patients who would benefit from one-on-one assessment and intervention from specific prehab disciplines based on individual needs and circumstances. Examples include, but are not limited to smoking cessation, weight-loss, pain management issues, need for additional supports at home following surgery, pre-operative strengthening programs, etc.
Your orthopaedic surgeon has the expertise to replace your worn and damaged joint, but you have the most important role to play in your surgery and recovery.
You must prepare to achieve the best possible outcome from your surgery. Here is what you can do to get ready for that big day:
- Follow your orthopaedic surgeon’s recommendations
- Your surgeon and his office give you specific instructions to follow that are important to your health and safety leading up to and including your surgery. Not following these recommendations can cause your surgery to be cancelled at the last minute or unnecessary complications to happen.
- Maintain or improve your fitness level and your joint range of motion – maintain strength and mobility.
- The healthier you are going into the surgery, the more efficient your recovery will be.
- Maintain or attain a healthy weight.
- People who are overweight have a higher risk for complications after surgery.
- Have any dental work done.
- Having dental work done before surgery reduces the risk infection after surgery. This is especially true for major dental procedures.
- Learn about your surgery.
- Seek out information and ask questions, however, be careful to ensure that the information you review is credible.
- Talk to people who have had a similar surgery (visit Orthoconnect).
- People’s experiences can ease your mind or worry, but be sure to remember that everyone is different and that not all people have the same interpretation of their experiences.
- Prepare yourself and your home:
- Stock the freezer with quick and easy to prepare meals.
- There are many things to do around your home in preparation for surgery, making easy meals for yourself, and setting up a bedroom on a main floor are some examples of things that are helpful in easing your transition from hospital to home. Your therapist will assist you in determining what needs to be done to get your home environment ready ahead of time.
- Quit smoking at least two weeks prior to surgery to reduce complications and aid soft tissue and bone healing.
- Smoking is a lifestyle habit that is difficult to change, however your risks of complications are greatly reduced if you do not smoke. Consider your options and talk to your family doctor about quitting smoking as there are many methods to help you succeed.
- Find out how long you may require outpatient physiotherapy and locate a physiotherapy facility close to home. (Manitoba Physiotherapy Association website)
- In Manitoba, access to physiotherapy services beyond those offered to you in the hospital is variable. However, there are many ways to obtain the rehabilitation you require. Be sure to discuss your needs and services with your therapist before and during your hospital stay.
- Find out what, if any, assistive equipment you’ll need to rent/purchase.
- Things you can do now and will be able to do again may be difficult for a while after surgery. You will need an assistive walking device such as a cane or walker and other equipment such as a shower chair, grab bars and raised toilet seats. Talk to your therapist about these devices and how to arrange to get them.
- If your recovery involves not bearing weight on your limb, consider practicing using crutches or a walker to test your ability to comply with the requirements during your recovery. If you are not able to remain off of your affected leg, you may need to prepare to have more help, such as a wheelchair or assisted-living environment to recover until you are told that you may put full weight on your leg again.
- Arrange any supportive care (including a driver), if needed, in preparation for discharge from hospital.
Your surgery date is drawing near and you have had your pre-op medical check-ups completed and visited the pre-admission clinic. But there are still things to do. Below is a basic checklist to help you prepare for surgery and for the recovery period afterward:
Household
- Put things in order and tidy up
- Organize a “recovery room” for your return after surgery (make a bed on the main floor, move a firm arm chair to the main floor, have several pillows ready, make room for use of a walker in the house)
- Remove area rugs that could cause a fall
- Remove electrical cables that could cause a fall
- Prepare/buy easy-to-prepare dinners
- Arrange a ride to and from hospital and therapy visits
- Pack bag for hospital
- Get special equipment recommended by the therapist (bathroom grab bars, bath seats, raised toilet seats, long handled reachers and shoe horns, elastic shoe laces, handheld shower)
- Identify local pharmacy and grocery stores with delivery service
What to Pack
- nightclothes
- dressing gown and slippers with closed heel and toe
- loose clothing that are easy to put on
- walking or running shoes
- eyeglasses and or hearing aids
- personal care items
- all your medications in their original containers
- books and magazines
- Note: Leave cash, credit cards, jewelry, CD players and other valuables at home.
Medication List
- Medication
- Reason
- Dose
- How Often
Personal Grooming Checklist
- toothbrush/toothpaste
- hairbrush/comb
- eyeglasses/contacts
- deodorant
- shampoo/conditioner
- razor
- feminine hygiene products
- skin lotion
Rehabilitation
Your date for surgery has arrived! You will have received instructions from your doctor about when to stop eating and drinking in preparation for surgery. If you take daily medications, especially blood thinners, ask during your Pre-Admission Clinic visit if you should still take them the morning of surgery. While each hospital may have variations, the basic processes are the same.
You arrive at the hospital about 2 to 2½ hours before your scheduled surgery time and report to the Pre-Operative or Pre-Admission Clinic. Staff will provide you with hospital clothing, an identification wristband, and an explanation of what to expect in the surgical area. Staff may also ask some questions about your medical history and check your temperature, pulse, respiration, and blood pressure.
For your peace of mind and safety, make sure that you know which joint or limb will be undegoing the surgery. Check that the nursing staff and surgeon are in agreement. A representative of the surgical team will sign his/her initials on the appropriate place before the surgery.
Check that the consent lists the correct surgery that you are having. You will have an intravenous (IV) line started to provide fluids and medications during surgery. The anaesthetist will likely speak with you just prior to surgery.
The Surgery
In the Operating Room, you will be prepped for surgery. The type of anaesthesia discussed with you will be given and surgery done. Skin will be cleansed and all areas except the surgical area will be covered with drapes. The length of time the surgery takes depends on the surgery being performed. You may have a bladder catheter inserted to drain urine.
Following your surgery you will be taken to the Recovery Room or Post Anaesthesia Care Unit to have your blood pressure, pulse and breathing checked. You will receive medication for your pain either intravenously or by injection. You will be asked to do your deep breathing and possibly some exercises to ensure good circulation. You may have an x-ray taken.
Approximately 2 hours following your surgery, you will be moved to your room. At that time, the nurse will assess the wound dressing and medications you normally take may be restarted. You will receive medication to control your pain which may be given by through the IV, injection or as pills. You may have clear fluids and possibly some toast if you wish. The surgeon will speak to you or your family about the surgery.
Your Recovery
After surgery, the focus is on your comfort, healing and recovery. Minimizing pain and preventing complications are critical to all three.
Patients are ready for discharge home once the following criteria are met:
- you are medically stable (vital signs stable, voiding on own, no nausea and vomiting, your pain is controlled and you are tolerating your diet)
- you are able to manage activities of daily living, dressing, bathing, toileting (some patients will require home care as per Occupational Therapy assessments)
- you are able to mobilize independently, you can get in and out of bed on your own, on and off the toilet on your own, you can walk independently the distance required for each individual, and you can manage stairs if required
- you can administer your blood thinner, dalteparin (Fragmin), acetylsalicylic acid (aspirin) or rivaroxaban (Xarelto) for 28-35 days for hip patients or 14days following discharge for knee patients
- for certain low-risk patients, hip replacements can now be done as outpatient procedures, meaning that the patient can go home on the same day as the surgery
All surgeries come with a risk of complications; they are not common, but they can happen. The complication rate following joint replacement surgery is low. Different people react to complications differently both physically and emotionally. Being aware of your tendencies for reaction will help understand and deal with complications should they occur. Chronic illnesses (diabetes, heart or lung disease) may increase the risk so a complete evaluation of your health is required before your joint replacement to determine your fitness for surgery. By following your doctor’s orders and knowing the possible complications you can do a great deal to prevent or lessen complications.
Low Blood (Anemia)
Depending on the type of surgery you have, you may lose a significant amount of blood. Blood loss can result in a drop in your haemoglobin; this is called anemia. Haemoglobin carries oxygen throughout your body and can be measured with a blood test. If your haemoglobin level is too low, you may feel dizzy and weak, short of breath, nauseous and very tired and you may have a headache. You may require a blood transfusion.
You may prevent low blood and a blood transfusion by:
• Following Canada’s Food Guide for healthy eating.
• Having a complete blood count (CBC) at least 3 months before you come to the hospital and follow-up with the results of your test. Ideally your haemoglobin level should be in the high end of the normal range.
• Consulting with your family doctor about the need for iron, or vitamin supplement.
Blood Clots
Blood clots can develop in the deep veins during the first several weeks after surgery. These blood clots could dislodge and travel to the lungs causing serious health risks. If you already have problems with your heart or circulation, are inactive, overweight or have other health problems such as diabetes or cancer you have a greater risk of developing blood clots. Let your surgeon know before surgery if you have had a clot in the past.
You can prevent blood clots after surgery by:
• Getting up and moving frequently. Every hour, pump your feet and ankles; and tighten and release the muscles in your legs and buttocks.
• Wearing leg support stockings while you are in bed in the hospital if your doctor feels you need them.
• Taking blood thinners (anticoagulants) as prescribed by your surgeon. Blood thinners are used to prevent clots after a major operation on your legs, such as a hip or knee replacement. The number of days you require this medication depends on your risk and is decided by your surgeon. Blood thinners vary in preparation and may be in pills or by injection. Your surgeon will determine with you the best option for your particular circumstances. Oral medicines are taken as a pill or capsule. Some oral medicines require blood monitoring to ensure they are not interacting with foods and other drugs, and to ensure the correct dose; others do not. Injectable medicines are given as a small injection under the skin of the abdomen. They are administered once or twice daily, and the hospital nurses will teach you or your support person how to use these medications so you can manage at home.
Infection
Less than one percent of patients develop a wound infection after surgery. However, when infection occurs, it is a very serious complication – so prevention is key. Infections can start in your joint during surgery, in the hospital or when bacteria travel there from elsewhere in your body. You are more likely to get an infection if you are not well nourished or if your immune system is not strong (such as with diabetes or rheumatoid arthritis).
You can prevent infection by:
• Getting your body in shape by eating healthy foods before and after your surgery
• Taking the antibiotics you will receive after surgery
• Washing your hands frequently
• Following carefully instructions for wound care
• Avoiding people who have colds or infections
• Stop smoking before your surgery
• Talking with your physician if you suspect or see signs of an infection
Signs of an infection:
• Fever
• Redness or swelling of a wound
• Drainage from a wound
• Increased pain in the surgical area during activity and rest
The symptoms of an infection may also be signs of a hematoma (bleeding into the tissues around the surgery). Alert your health care provider if you experience these signs; it is very important to talk to your health care provider as it is important to differentiate between the two conditions. Be sure to notify your dentist and other doctors if you’ve had a joint replacement. Even during a routine dental examination, you might run the risk of an infection. A small infection can be a major problem, and your health care professionals know what precautions to take. It’s up to you to keep them informed.
Dislocation
Dislocation occurs when the ‘ball comes out of the socket’. This occurs in 1-2 % of cases although the risk can be dramatically higher in cases of revision. The risk of dislocation is greatest just after surgery as the tissues (muscles, ligaments) around the new joint are not fully healed. However a small risk is always present after this type of operation. The signs of dislocation are sudden, sharp, severe pain and a shortened leg. If dislocation occurs, a hospital visit is required to relocate it. This can usually be done without opening the joint surgically. After this you may require a brace for a few months.
You can help to prevent dislocation by:
• Consistently and carefully follow the activity guidelines and precautions provided to you by your health care team. (avoid, twisting the hip, crossing the legs and bending the hip past 90 degrees towards your chest)
• Obtain and use the assistive equipment (long-handled reachers, shoe horns, raised toilet seats) prescribed for you by the physiotherapist and occupational therapists.
Leg Length Difference
It is common to have up to a 1cm leg length difference after hip replacement. This difference is to ensure there is enough tension in the muscles around the hip to prevent the hip from dislocating. At first you may feel you have a longer leg and find yourself limping, but with walking and exercise, the sense of imbalance will often pass. A small number of patients may require a shoe lift placed either within or to the sole of their shoe, depending on the size of the lift required.
Persistent Limp
A small number of patients can have a persistent and sometimes permanent limp after joint replacement surgery. There are many causes of ongoing limp including pain, arthritis elsewhere in the body, persistent muscle weakness around the hip, leg length discrepancy, and nerve injury. If the leg length difference or limp is bothersome to your recovery, speak to your therapist or doctor about it. In some cases, additional therapy or surgery could be required to address the underlying cause of the limp.
Swelling
You may experience significant swelling in the affected limb for the first few weeks after surgery. To help reduce the swelling, elevate the affected limb, ideally 8 to 12 inches above the level of the heart, whenever possible. If the affected limb is your leg or foot, avoid sitting for long periods and pump your feet and ankles to keep your circulation going. Swelling is often on of the last symptoms to resolve after surgery and may be present for up to 12-18 months following surgery.
Respiratory or Lung Complications
Lung complications such as fluid in the lungs or pneumonia may occur due to the anaesthetic and prolonged bed rest.
To prevent them:
• Do not eat or drink after midnight on the night before your surgery.
• Get up and move, change your position in bed frequently.
• Take 10 big deep breaths and cough every hour on the days after your surgery.
• Quit smoking at least two weeks prior to surgery.
• If there are any problems with breathing or shortness of breath, see your health professional as soon as possible.
Cardiovascular
The two most common postoperative heart complications are heart attack and heart failure. The stress of surgery can cause a heart attack in people with coronary artery disease, which may or may not have caused symptoms before the surgery. In and extremely small number of patients, this can result in death. Be sure to inform your surgeon and anaesthetist about your cardiovascular health and follow their instructions.
Delirium after surgery
Sometimes older people go through a period of confusion or delirium after surgery. They may act or talk in ways that are not normal for them. For example, they may become forgetful, mixed up, and or see, hear and believe things that do not make sense. Delirium usually goes away in a few days but sometimes lingers for a few weeks. Delirium is usually due to more than one cause. Some common causes of delirium are: side effects of anaesthetics and medications, lack of sleep, pain, infection, alcohol withdrawal, constipation and low oxygen levels. The health care team looks for and corrects the cause of the delirium whenever possible.
Urinary Retention
The inability to urinate (go to the bathroom) is a very common problem following any type of surgery. The problem is relieved by passing a catheter (tube) into the bladder and draining the urine. The catheter may be left in place for several days or removed immediately after the bladder has been emptied.
Nausea
The most common postoperative complication is nausea. Intravenous hydration (fluid through the IV tube) is often all that is required. If nausea and vomiting continue, medication may be given. You are given clear fluids after surgery to make sure you are not nauseated; once your stomach is working, you will be moved on to your normal diet.
Constipation
Lack of activity following surgery and the use of narcotics, which control pain but also reduce bowel function, is usually the cause of constipation. If needed, stool softeners and laxatives may be prescribed.
Antibiotic Diarrhea
Antibiotics given to the patient around the time of surgery for prevention of infection in the surgical wound, may result in diarrhea. This occurs when the natural bacteria in the bowel or intestine are killed off by the antibiotic and other bacteria become more plentiful. The patient may require replacement of fluids by intravenous for a few days if the patient becomes dehydrated.
Allergic Reactions
There may be allergic reactions as a result of the medications you have been prescribed. The most common is a reaction to penicillin or sulpha drugs. Reactions can vary from a mild rash to an intense life-threatening reaction. Be sure to tell your doctor about any previous allergic reactions. If you suspect you are having an allergic reaction, inform the nurse immediately.
Skin Complications
Bed sores may result from pressure on the skin over bony parts of the body in patients who are in bed for long periods or in a poor state of nutrition. This condition can be prevented using good skin care techniques, a sheepskin cover on the bed, or devices to raise the affected area off the bed.
Nerve Injury
Depending on the surgical area, nerve injury may result due to the proximity of the nerves and blood vessels. Usually the result is temporary especially if the nerves have been stretched by retractors holding them out of the way. Permanent injury is rare.
Vascular Injury
There is a small risk of injuring a major blood vessel to the leg. This can result in major blood loss and well as loss of blood flow to the portion of the leg below the injury. This could require additional surgery to be performed by a vascular surgeon and, in vary rare circumstances, can result in the loss of the leg.
Fractures
Sometimes when inserting the prosthesis into the bone, the bone may break. This is a more common complication of revision joint replacement or in those with thinning of the bones (osteoporosis). If this does occur it is often recognized during the surgery and is treated immediately. If you have a fracture there may be a period of time when you will not be allowed to put all your weight on your operated leg.
Hematoma
Bleeding (hematoma) may occur in the muscles around the hip joint following the operation. If a hematoma occurs, a bruise may be visible or the area may be red, hot and swollen. In some cases, the hematoma may need to be drained, otherwise the body will absorb the blood naturally. Exercise and therapy usually help remove excess blood.
Misalignment or loosening of the prosthesis
One or both parts of your new joint may loosen with time or can sometimes fit imperfectly during surgery. It is important to follow the activity guidelines and attend all follow-up appointments with your surgeon so that the alignment and fit of the new parts can be monitored by the surgeon.
Stiffness
A knee joint may stiffen after surgery. Patients who have stiff knees before surgery are more likely to have this problem. It is important to maintain your flexibility while awaiting surgery to reduce the risk of stiffness following the operation. This can be done through exercises provided by a physiotherapist. Manipulation (stretching of the joint) may be required to correct stiffness after surgery.
Pain, Swelling and Fluid in the Knee
It is common for knees to have some swelling, be red and warm after surgery. This may last several months. This is different from infection which causes a sudden increase in pain, swelling and stiffness as well as fever and chills.
After a hip replacement the muscles and tissue around the hip take time to heal. Your surgeon will assess the inherent stability of the hip during surgery. Depending on the assessment, your doctor may recommend avoiding certain movements for 3 months following your surgery to reduce your risk of dislocating your new hip.
1. Do not bend your hip past 90˚
Below are shown INCORRECT positioning of the hip: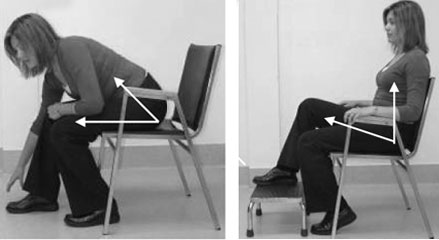
When sitting, do not bend forward, or sit with your knees higher than your hips. When standing do not bend past 90˚ at your hip. Your therapist will teach you ways to avoid these positions during our stay in hospital.
**Tip: You want to avoid your thighs getting close to your chest. It is important to think of your body in space as the 90° angle looks different in sitting, standing and when lying in bed.
2. Do not cross your legs at the knees or at the ankles.

When standing do not bend past 90˚ at your hip. Do not cross your legs at the knees or at the ankles.
• Do not let your operated leg cross the midline of your body.


• A general rule to remember is to keep your feet at least shoulder width apart.
• You will have to keep a pillow between your legs in bed to ensure your operated leg doesn’t come to the midline.
3. Do not twist your body or turn your operated leg inward.

• Take small steps when turning.
• Do not pivot. (turn on a planted leg)
When resting or elevating the leg after knee replacement to control swelling, be sure to elevate the entire leg and do not lie with a pillow under only the knee so that the knee is bent. The leg should rest in a straight position.
Surgical Team
Other Treatment Options
Hip FAQs
Knee FAQs
Downloads
In this section we have compiled information and made them available for downloading as PDFs. If there’s something specific you’re looking for/can’t find, please contact us.
From Winnipeg Regional Health Authority:
Patient Hip Information Manual
Patient Knee Information Manual
From the Canadian Orthopaedic Foundation:
Planning for Maximal Results – Preparing for Surgery
Get Moving: Maximizing Your Activity After a Hip or Knee Replacement